Nicolette, Inc., a digital health pioneer focused on patient education and data tools
Continue readingHe lost his baby daughter. Then he turned his grief into a tool for NICU parents.
NicoBoard is an app that helps parents make sense of a frightening time.
Continue readingHow Innovation Can Empower Patients and their Families
Have you ever wondered if a past event could have turned out differently if you had additional knowledge, experience or tools?
Continue readingA new tool to empower CHOC NICU parents
Parents of patients in the neonatal intensive care unit at CHOC Hospital now have at their fingertips new technology to help them better understand, track and analyze data showing their baby’s progress while receiving care.
Continue readingNicolette, Inc. Launches Patient Empowerment Technology for NICU Parents
Choosing Value Over Volume
If it feels like you’re paying a much higher price for the same healthcare than you were a few years ago, you’re right.
And you’re not alone.
Healthcare spending at the individual and government level has increased exponentially in the past decade, as shown below.
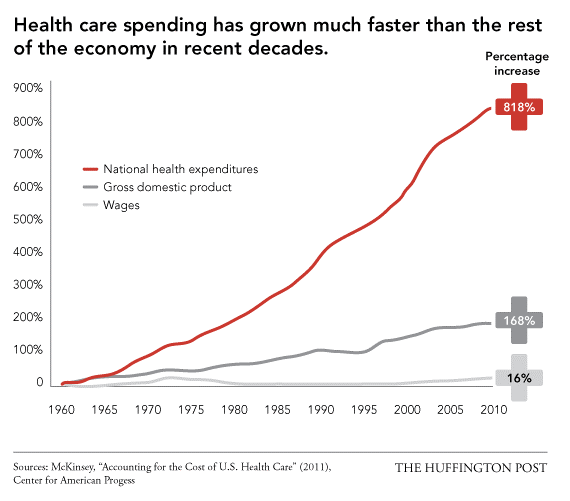
From providers to payers, innovators to government officials, many in the U.S. healthcare community are finding that these increasing costs are not always improving patient outcomes. As a result, the healthcare space has been gradually undergoing a paradigm shift for the past few years: moving from healthcare that is volume-based to value-based.
Quality Versus Quantity
The difference between the two is in how hospitals and physicians are reimbursed by insurers for their services. In volume-based healthcare, providers are paid fee for service, based on how many times they treat patients, as opposed to how beneficial those treatments are.
In value-based healthcare, as the name suggests, providers are reimbursed based on the value their treatment brings to the patient, as opposed to just the treatment itself. Payments are based on patient health outcomes. Providers are rewarded for helping patients improve their health, reduce the effects and incidence of chronic disease, and live healthier lives in an evidence-based way.
Driving the Change
Currently, insurers are the primary drivers of this change. The CMS (government body that oversees Medicare and Medicaid) now allocates $2 billion dollars annually for value-based reimbursements2. Other private insurers such as Blue Cross Blue Shield and Aetna are following suit by pledging certain percentages of their budget for value-based systems3,4. These insurers have their own metrics and surveys (you may have heard of HCAHPS) to assess hospitals’ achievements in areas such as mortality and complications, patient safety and experience, and efficiency and costs of processes. How much the insurers reimburse is then reflected by how much value hospitals bring to each of these areas.
The Future of Value-based Healthcare
In this next decade, emerging technology will play a huge role in helping insurers and providers usher in this value-based system. Below are some examples of these technologies that are currently being developed:
• Telemedicine and wearables are allowing providers to more closely and consistently monitor patient health, without the associated costs of seeing them at a hospital or clinic.
• Machine learning algorithms are analyzing large sets of health data to aid physicians to identify issues before they even happen, shifting the focus to cheaper preventative medicine.
• Improvements in healthcare IT are bridging the information gaps between physicians, patients, and insurers, providing data-driven insights into which specific areas in the healthcare system can be improved to provide more value.
Technology is changing this medical landscape as we know it. But the future of value-based healthcare also depends on a confident and informed patient. This is a patient who creates personal health data, is aware of what they want out of their healthcare, and actively engages in healthcare discussions to voice these values (more on this here). A value-based system has no meaning until patients come together with providers and insurers to arrive at a shared definition of valuable healthcare. So, as you navigate your health journey in this increasingly value-based system, know what you value and share it.
1.The Huffington Post. “Why US Healthcare is Obscenely Expensive”. 2013. Web.
2.US Centers for Medicare & Medicaid Services “CMS Hospital Value-Based Purchasing Program Results for Fiscal Year 2018”. 2017. Web.
3.Blue Cross Blue Shield. “Blue Cross and Blue Shield Companies Continue to Lead Nation’s Path to Value-Based Healthcare”. 2015. Web.
4.Aetna. “Joint ventures improve member care, reduce costs”. 2018. Web.
Take Charge of Your Health
Don’t be a passive patient.
Truly personalized medicine depends on one agent of change: the patient. Leading your own healthcare journey depends on taking actions. Taking action takes confidence and persistence. Here are some essential steps we recommend to get going and stay the course:
The obvious big picture goal is to recover and live your healthiest life possible. But this overarching aim to just “get better” can sometimes be impersonal or out of scope. Add personal meaning to goals by making them more specific to how they will improve your life. From there you can drill down into the numbers that need to change.
Take the example of high blood pressure. Current target guidelines are below 120 over 80. If your blood pressure is moderately above this guideline, say 128 over 85, it’s simple to acknowledge that it’s high and needs to come down over time. However, it likely doesn’t inspire a consistent and rigorous commitment to actions on a daily basis.
By contrast, translating high blood pressure to life is very inspiring, as it leads to issues such as:
- Increased risk of heart attack, stroke, vision problems, and sexual dysfunction
- Higher susceptibility to negative health events due to stress or rigorous activity
- Greater difficulty in returning to normal levels as one ages
With this knowledge, ask yourself: what about lowering your blood pressure means the most to you? As a result, your true goals may look like these:
- I want to look and feel great at my kids’ weddings
- I want to run a marathon
- I want to have a great sex life as I get older
- I want to take the risk of starting a business and be healthy enough to handle the stress
Getting below 120 / 80 now means a lot more.
Now it’s time to get into the concrete details. Work with your healthcare team to come up with the highly-specific actions that will get you to your goal. High specificity makes the actions easy to track and simple to commit to. For high blood pressure, these might be along the lines of:
- Eliminate soda from your diet
- Walk or jog 3 miles per day
- Meditate for 15 minutes each morning
- Eat something green at both lunch and dinner
These are simple to comply with because they form a checklist that can be tracked each day. Contrast this with the less specific idea of “eating healthier” or “getting exercise”. These are not wrong, but impossible to track and hence know whether what you are doing is working.
You can use pencil & paper, a spreadsheet, or even a digital health app (our favorite). No matter how you do it, it’s critical to document two things:
1. Actions taken
2. The metric you are improving
In the case of blood pressure, you would document whether you complied with no soda, greens at lunch & dinner, meditation, and distance of your walk/jog. Since these are daily actions, you would track them every day. At the same time, you would measure your blood pressure frequently and establish a trend.
Tracking actions and metrics empowers you in the following ways:
- Understanding what works: You need to know if your prescribed actions are working for you. If it’s been one month and the needle isn’t moving on blood pressure, additional actions may need to be taken. On the flipside, if it’s working and you’re feeling good, perhaps you can do more, like run faster and farther.
- Compliance checking: Keep yourself accountable for sticking with your goals. Without documentation, it is easy to trick yourself into believing that you’ve made changes that you actually haven’t. It’s important to know that if the desired effects are not happening whether it’s because you need to try something else or you haven’t been complying with what you originally set out to do.
- Motivating yourself: Making positive changes are not naturally easy, at least not in the beginning. The first few days can feel like an eternity, especially if the results aren’t showing up right away. Recording the daily victories when you accomplish your goals makes every win real, and can help motivate you to stay on track.
Your healthcare journey is much easier and enjoyable when shared with others. There are many individuals around you that can and want to be a part of it. Take the initiative to reach out to the following networks for support along your journey.
- Healthcare team: These are your medical experts and know the technicalities of your health goals. You need them to provide their medical experience and knowledge as much as they need you to provide your expertise in yourself and your body.
- Family and friends: They may know things about you that are not apparent to yourself that can help you on your health journey. Perhaps they’ve noticed changes in behavior or attitude as a result of high blood pressure that you haven’t realized yourself. Reach out to them for a second opinion or as your social support system to guide and empower you.
- Other patients: No one patient can know all resources and research available to them. Luckily, there is a high chance that there are other patients going through what you are going through. Plenty of online and in-person patient communities, like this, exist where stories and experiences are shared. Utilize this collective knowledge to enable you to make more informed medical decisions.