Parents of patients in the neonatal intensive care unit (NICU) at CHOC Hospital now have at their fingertips new technology to help them better understand, track and analyze data showing their baby’s progress while receiving care.
Launched at CHOC in fall 2020, NicoBoard is a tablet-based application that translates a stream of numbers pulled from their baby’s electronic medical record – data such as body temperature, weight gain and loss, feed volumes and more – into easily understood, simple sentences complemented by visual aids like graphs and charts.
Coupled with curated education and research materials, this helps parents better analyze trends and track progress, enhancing decision making and supplementing the detailed conversations they have with their baby’s care team at CHOC.
The system also provides parents with an outlet for journaling so they can document their baby’s experiences and milestones to remember later.
“At CHOC, we are fully committed to patient- and family-centered care, and families play an integral and active role in their child’s care plan,” said Jennie Sierra, NICU nursing director. “These tools build upon that commitment, further helping our families better understand complex medical data, stay engaged and ask important questions.”
A personal experience sparks an idea
The platform was developed by the father of two CHOC NICU patients who found himself searching for a tool that would help him better make sense of the data being reported on his children during their hospital stay.
Phil Martie’s twins, Bexley and Nicolette, were born in 2014 at just 25 weeks gestation. What would follow was a 110-day odyssey that would change Phil’s life forever.
After almost four weeks at another hospital, the Martie twins were transferred to CHOC. Upon admission, physicians there found that Nicolette had a hole in her intestine. Surgery was ordered immediately to repair the perforation, but Nicolette heartbreakingly passed away during a four-hour procedure.

Bexley gets a bath as a baby
Bexley’s journey included battles with sepsis and a heart problem called patent ductus arteriosus, wherein a connection between the aorta and pulmonary artery that’s open during gestation fails to close shortly after birth and requires surgery. He also needed to grow, learn to eat by mouth and gain strength in his body.
Between the procedures, medications ordered, physical and feeding therapy, and day-to-day care in the NICU, Phil was struck by how much data and information he received about his children and how difficult it was to process that intel – especially while feeling the stress so common to many NICU parents.
“At CHOC, they gave all the access to data and information we ever wanted, but there’s still so much data that’s generated by the baby,” founder Phil Martie says
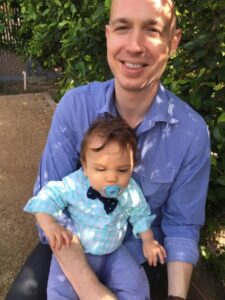
Phil and Bexley
That no tools seemingly existed to help solve this problem planted a seed for Phil, who had a background in business process improvement.
A desire to support a community of fellow NICU parents nurtured that seed, and a few years later, NicoBoard sprouted through Phil’s new company – Nicolette, named after Phil’s late daughter.
Today, Bexley is a happy and healthy 6-year-old. He was discharged from CHOC around his original due date without the need for medical equipment. Bexley likes to say he works at Nicolette, his dad says.

Today, Bexley is a happy and healthy 6-year-old
“I had this deep experience that lasted 110 days that included death and success – two different outcomes and textures,” Phil says. “The NICU experience is very textured. I’m in a unique position to do something – it’s a privilege.”
Another addition to a high-tech NICU
NicoBoard is among a host of advanced technology offerings in CHOC Hospital’s level 4 NICU, a 24,000-square-foot, state-of-the-art facility with 36 private rooms.
CHOC Hospital offers special units within the NICU to provide highly customized care for babies, including a small baby unit for children born between 24 and 28 weeks gestation or who weigh less than 1,000 grams; babies who need complex surgery; and babies who have neurological and cardiac concerns.
